Tarsal Tunnel Syndrome: A Complete Guide
By Yuna Zhuang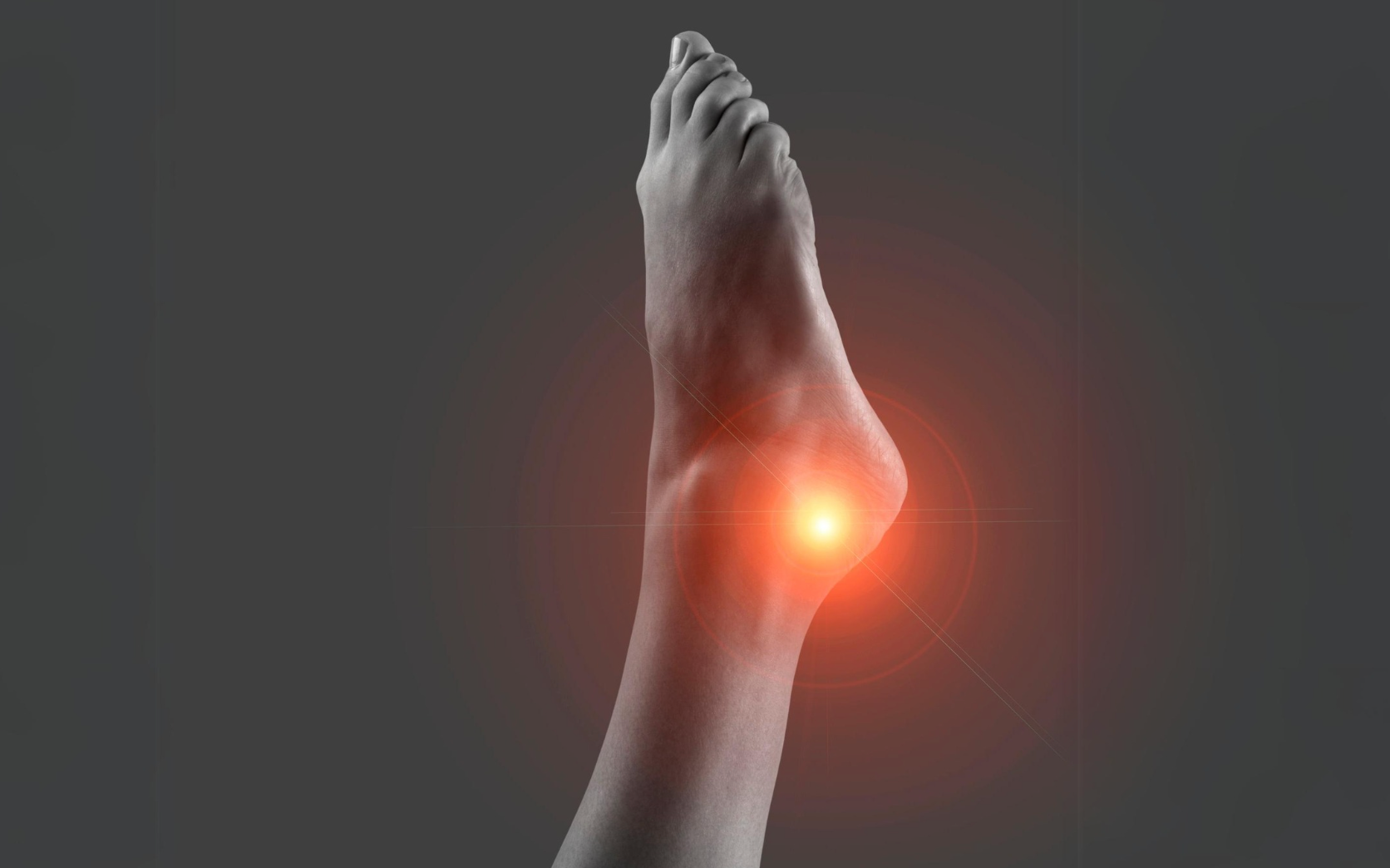
The tarsal tunnel is made up of the ankle bones and a band of ligaments that stretch across the foot. It contains many nerves, blood vessels, and tendons that help the foot move and be flexible. When the posterior tibial nerve is compressed, often due to overuse injury, it can lead to Tarsal Tunnel Syndrome (TTS).
This foot condition results from nerve compression and pressure in the ankle area, causing chronic pain and discomfort. Not many people get a formal diagnosis of TTS, so there isn't a precise number of its prevalence. However, existing diagnoses indicate that people over 20 are prone to this condition. Additionally, nearly 60% of TTS clinical cases often occur without a clear cause, which makes this condition more unidentifiable.
In this guide, we'll cover everything about Tarsal Tunnel Syndrome, from the anatomy of the tarsal tunnel to causes, symptoms, and treatment options. We'll also get a comprehensive look at what to expect with TTS and how to manage it.
Where Is the Tarsal Tunnel in Your Foot?
The tarsal tunnel is a narrow, tunnel-like structure located along the inner side of the ankle and foot. Protected by the flexor retinaculum—a strong, thick ligament—the tarsal tunnel houses several important structures, including the following:
- Posterior tibial nerve
- Arteries
- Veins
- Tendons (tibialis posterior and flexor hallucis longus)
The posterior tibial nerve, which runs through the tunnel, is the primary nerve involved in TTS. It has two branches: the lateral plantar nerve and the medial plantar nerve. These nerves have specific roles in supplying sensation and motor function to the foot, and their compression can lead to various symptoms associated with TTS.
Similar to carpal tunnel syndrome in the wrist, tarsal tunnel syndrome arises when the posterior tibial nerve undergoes excessive pressure or compression, often due to injury or anatomical factors.
What Is Tarsal Tunnel Syndrome (TTS)?
Tarsal Tunnel Syndrome is also known as Posterior Tarsal Tunnel Syndrome or 'posterior tibial nerve neuralgia.' It occurs when the posterior tibial nerve, along with the medial and lateral plantar nerves, becomes compressed within the tarsal tunnel. This nerve entrapment leads to symptoms that can range from mild discomfort to severe pain and nerve damage, affecting nerve and muscle function in the affected foot. As a result, you may find yourself having difficulty when performing physical activities.
It's Not Plantar Fasciitis
Tarsal tunnel syndrome is often mistaken for plantar fasciitis, another common source of foot pain. However, plantar fasciitis is inflammation of the plantar fascia, a ligament on the sole of the foot, rather than the nerve compression that characterises TTS. In short:
- Plantar fasciitis involves inflammation.
- Tarsal Tunnel Syndrome involves nerve entrapment within a confined anatomical space.
Who Has Tarsal Tunnel Syndrome?
Tarsal Tunnel Syndrome can affect people of all ages, but common findings indicate prevalence among young adults in their 20s. This condition is also often seen in individuals who overuse their feet, such as athletes, those with flat feet, or individuals with other foot conditions.
Certain underlying conditions, like ankle sprains, tarsal coalition, or structural abnormalities in the ankle bones, can also increase the risk of developing Tarsal Tunnel Syndrome.
Symptoms of Tarsal Tunnel Syndrome
Tarsal Tunnel Syndrome symptoms may vary in intensity but often include:
- Burning sensation in the ankle or foot
- Numbness or tingling along the inner ankle and plantar foot
- Sharp pain that may worsen with prolonged standing or walking
- Swelling or a feeling of fullness in the ankle area
- Pain extending to the toes and heels, more often at night
- Difficulty standing for extended periods
What Causes Tarsal Tunnel Syndrome?
TTS results from pressure on the posterior tibial nerve within the tarsal tunnel. Two in five patients associate TTS with ankle injuries, such as sprains. Other contributing factors may include:
- Structural abnormalities, such as flat feet, tarsal coalition, or bone spurs.
- Swollen tendons or soft tissue stress, with tendonitis or ganglion cysts encroaching upon the tarsal tunnel.
- Overuse injury, including excessive standing, running, or other activities.
These factors are common among nerve entrapment syndromes, including the Anterior Tarsal Tunnel Syndrome (ATTS), a compression of the deep peroneal nerve.
How Is Tarsal Tunnel Syndrome Diagnosed?
An accurate diagnosis is essential for effective treatment of TTS. There are numerous foot and ankle injuries and conditions, each targeting distinct parts. Unfortunately, not all sufferers of TTS undergo proper diagnosis.
To diagnose Tarsal Tunnel Syndrome, foot and ankle surgeons or physiotherapists typically conduct a physical examination first thing to check for tenderness and assess joint mobility. They also perform nerve conduction studies to evaluate tibial nerve function and detect compressive neuropathy. This is also known as the Tinel’s test.
For detailed images of the soft tissues and bones, imaging tests, such as Magnetic Resonance Imaging (MRI), help for further assessment. Your healthcare provider will examine muscle atrophy and structural abnormalities around the tarsal tunnel.
Treatment for Tarsal Tunnel Syndrome
Treatment for Tarsal Tunnel Syndrome can range from conservative methods to surgery, depending on the severity of symptoms and response to initial treatments. Below are two methods to address and treat Tarsal Tunnel Syndrome.
Non-Surgical
Minimally invasive treatments focus on relieving symptoms and preventing further injury, including ankle sprain physiotherapy treatments. Ankle sprains, being one of the major culprits of TTS, can be prevented with the proper treatment plan.
Physiotherapy providers in Singapore, like Phoenix Rehab, tailor personalised plans for TTS. This involves exercises like tibialis posterior strengthening, calf stretching, and nerve mobility work to reduce pain and improve joint function. Physiotherapists may also recommend orthotic devices for certain cases. This device is a medial heel wedge or supportive arch that helps offload pressure on the posterior tibial nerve.
Upon the advice of healthcare professionals, steroid injections or corticosteroid injections can temporarily relieve inflammation, though repeated use may weaken the surrounding tissues. Anti-inflammatory drugs may also alleviate pain, but they don’t treat the underlying nerve compression.
These conservative treatments work almost all the time in managing TTS and most ankle and foot pain.
Surgery
Surgery may be necessary for severe symptoms or persistent pain. Tarsal tunnel release is the most common surgical procedure, which involves freeing the posterior tibial nerve from the surrounding compressive tissue. Surgery is typically reserved for cases where nonsurgical treatment has not provided adequate pain relief.
What You Can Do at Home
Managing TTS at home is possible. Here are a few tips:
- Reduce activity on the affected foot to minimize inflammation through rest and elevation.
- Apply cold packs on the affected area to reduce swelling and alleviate mild pain.
- Incorporate footwear adjustments with shoes that provide arch support and a roomy toe box.
Recovery Time
Recovery time from TTS treatments varies. For non-surgical treatments, relief can take several weeks, while post-surgery recovery may take several months, with physical therapy playing a key role in regaining strength and flexibility. The average recovery time is 6-8 weeks up to a full year.
What Happens If You Don’t Treat TTS?
Untreated TTS can lead to permanent nerve damage, muscle atrophy, and persistent foot pain. In severe cases, untreated TTS may cause tibial nerve dysfunction, leading to a loss of sensation or chronic weakness in the affected foot.
How To Prevent Tarsal Tunnel Syndrome
Even minor adjustments in your routine can go a long way to prevent TTS.
Avoid prolonged standing. Frequent breaks can minimise pressure on the ankle and foot.
Maintain joint mobility. Exercises focusing on foot muscles and ankle mobility help reduce the risk of nerve compression.
Strengthen surrounding muscles. Strengthening exercises for the tibialis posterior and calf muscles can improve stability and reduce stress on the tarsal tunnel.
When To See a Doctor
If you experience persistent foot and ankle pain, tingling, or burning sensations that do not improve with rest or home treatment, it’s time to consult a healthcare professional. Early intervention can prevent further injury and aid in a faster recovery.
What To Ask During Consultation
To make the most of your consultation, you may consider asking:
- What are the most effective treatments for TTS in my case?
- Are there specific exercises that can help with recovery?
- Should I consider orthotics or a particular type of footwear?
- What activities should I avoid during recovery?
Conclusion
Foot and ankle pain may feel like a normal condition, but without a formal diagnosis, it can get you into a complex situation. Tarsal Tunnel Syndrome can be difficult to manage without professional guidance, affecting your daily life and activities. Early diagnosis and treatment are key to preventing permanent nerve damage and reducing symptoms.
Browse other articles by category
Physiotherapy for Knee Pain Physiotherapy For Slipped Disc Physiotherapy for Neck Pain PHYSIOTHERAPY
PHYSIOTHERAPY
 Hand Therapy
Hand Therapy
 Alternative
Alternative
 Massage
Massage
 Traditional Chinese Medicine Treatment
Traditional Chinese Medicine Treatment
 Rehab
Rehab
 Physiotherapy For Lower Back Pain
Physiotherapy For Shoulder Pain
Orthopedic Doctors, Insurance & Healthcare
Physiotherapy For Upper Back Pain
Frozen Shoulder
Physiotherapy for Back Pain
Physiotherapy For Lower Back Pain
Physiotherapy For Shoulder Pain
Orthopedic Doctors, Insurance & Healthcare
Physiotherapy For Upper Back Pain
Frozen Shoulder
Physiotherapy for Back Pain
 Whatsapp us now
Whatsapp us now