Scoliosis Physiotherapy: What To Expect and How It Can Help
By Yuna ZhuangA noticeable curve in your spine (or someone else's) might be more than just a postural quirk. Scoliosis, often spotted in childhood or adolescence, can also show up quietly in adulthood. It affects how your spine moves, how your muscles work, and even how you breathe. For some, it’s a small curve that needs monitoring. For others, it’s a daily concern that impacts comfort and overall function.
The first step to managing scoliosis is to understand its nature, causes, and how it progresses. This includes learning about the different types, severity levels, and how scoliosis affects the body, patients, and even caregivers. In today's blog, we'll be covering these topics, which are especially useful when exploring non-invasive treatment options, such as scoliosis physiotherapy.
Definition of Scoliosis
Scoliosis is a condition where the spine curves sideways, rather than maintaining its typical straight alignment when viewed from the back. This sideways bend often appears in an “S” or “C” shape and may involve rotation of the vertebrae.
It may occur during growth spurts in adolescence or later in life due to spinal degeneration. While many cases are mild and manageable, others require closer medical attention, particularly if there’s significant curve progression.
Affected Anatomy
Scoliosis affects the spine, particularly the vertebrae, which are the small bones stacked to form the spinal column. In scoliosis, these bones curve sideways and may also twist, causing changes in spinal alignment. This abnormal curvature can strain the spinal muscles, affect the rib cage (especially in upper spine curves), and put uneven pressure on nearby joints and soft tissues. Over time, it may lead to muscle imbalances, reduced spinal mobility, and problems with breathing or posture.
Types of Scoliosis
There are several types of scoliosis, with the most common being idiopathic, congenital, and neuromuscular. Continue reading for a detailed look at the types.
1. Adolescent Idiopathic Scoliosis
Adolescent idiopathic scoliosis (AIS) is a sideways curvature of the spine that develops in children between the ages of 10 and 18, with no known cause. It's the most common type of scoliosis and is characterised by a lateral (sideways) spinal curve of 10 degrees or more. This type is often accompanied by vertebral rotation, and it occurs in otherwise healthy individuals.
Singapore has a measurable presence of AIS, particularly among school-aged children. Studies estimate that at ages 11 to 12, the prevalence of AIS is around 1.37% in girls and 0.21% in boys. These rates increase by ages 13 to 14, rising to 2.22% for girls and 0.66% for boys. This trend reflects the typical pattern of scoliosis onset during periods of rapid growth, especially in females, who are more prone to curve progression.
2. Congenital scoliosis
Congenital scoliosis is present at birth and results from a malformation of the spine during early fetal development. These structural anomalies may include abnormally shaped vertebrae or partial fusion of spinal segments.
Unlike idiopathic scoliosis, the cause is clearly structural and identifiable through imaging. The severity and pattern of the spinal curvature depend on the type and location of the malformation. Because the curve can worsen as the child grows, early diagnosis and regular monitoring are essential.
3. Neuromuscular scoliosis
Neuromuscular scoliosis develops in patients with underlying neurological or muscular conditions, such as:
- Cerebral palsy
- Muscular dystrophy
- Spina bifida
These conditions impair muscle control and balance, resulting in spinal instability and progressive curvature. Unlike idiopathic types, this form of scoliosis often involves a long, sweeping curve and tends to progress rapidly. It can also significantly impact lung function and sitting balance. Treatment focuses on maintaining comfort, mobility, and function, often involving physical therapy, custom seating, and in some cases, surgical intervention.
4. Degenerative scoliosis
From the word "degenerative" itself, this type is also known as adult-onset scoliosis, typically appearing in individuals over the age of 50 due to age-related wear and tear on the spine. It often results from the degeneration of intervertebral discs and facet joints, leading to spinal misalignment and asymmetrical load bearing.
Unlike adolescent forms, this type can cause significant pain, stiffness, and mobility limitations. Management often involves a combination of physical therapy, pain relief strategies, and lifestyle modifications. In severe cases, patients may require injections or surgery.
Mild, Moderate, Severe
The degree of spinal curvature in scoliosis helps identify an appropriate treatment plan. The severity can influence both physical symptoms and the risk of progression.
- Mild scoliosis
- Curves less than 20 degrees
- Often managed with physiotherapy scoliosis-specific exercises
- Moderate scoliosis
- 25–40 degrees
- May require bracing and structured exercise programmes
- At this stage, treatment focuses on stabilising the curve and preventing progression.
- Severe scoliosis
- Greater than 40–50 degrees
- Often monitored for potential surgical intervention
- Physiotherapy may still be part of the care plan to support mobility and manage pain.
How Common Is Scoliosis?
Scoliosis affects about 2–3% of the population. Adolescent idiopathic scoliosis is the most frequent diagnosis, particularly in girls aged 10–18. Adult scoliosis, especially adult degenerative scoliosis, is increasingly common with age-related spinal changes.
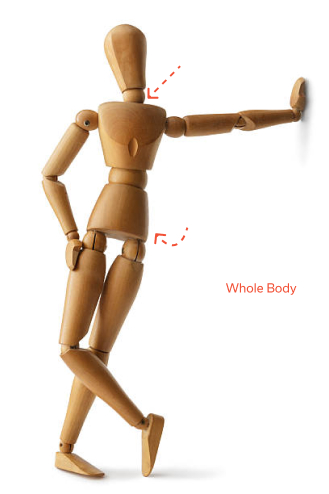
Symptoms of Scoliosis
Many children and teens with mild scoliosis show no symptoms or pain, making early detection challenging. However, there are subtle signs in posture, such as:
- Uneven shoulders or hips
- One shoulder blade that is more prominent or visible
- One hip appears higher than the other
- One side of the rib cage is elevated when bending forward
- Visible curvature of the spine
- Prominent ribs on one side
As the spinal curve becomes more pronounced, sufferers may experience back pain and noticeable changes in shape. In severe cases, the altered spinal alignment can exert pressure on the chest, potentially leading to difficulty breathing.
How Physical Therapy Helps With Scoliosis
Scoliosis physiotherapy supports the body in regaining muscular symmetry, improving posture, and reducing discomfort. Here are its key benefits:
- Alleviates pain and reduce muscle tension
- Slows or halt curvature progression
- Improves spinal health and flexibility
- Enhances postural awareness
- Strengthens supporting muscles
- Boosts confidence in movement and daily activities
- Delay or avoid the need for scoliosis surgery in some cases
In both adolescent scoliosis and adult cases, a personalised approach can make a meaningful difference in treatment outcomes.
How Scoliosis Physiotherapy Works
Scoliosis physiotherapy is a structured approach to improving function, posture, and comfort for people with spinal curvature. It’s not a one-size-fits-all programme. Instead, it’s a personalised plan built around the specific type and severity of scoliosis, as well as the patient’s age, symptoms, and daily challenges.
Physiotherapy doesn’t reverse the curve but can significantly slow its progression, improve spinal alignment, and support pain management strategies.
Objectives
The primary goal is to correct spinal abnormalities, restore balance in the body, and manage symptoms. Focus is placed on strengthening muscles, improving spinal alignment, and enhancing mobility while addressing the functional impacts of the spinal curve.
Assessment
Treatment begins with a detailed physical examination. A physical therapist will assess the following:
- Severity and flexibility of the curve
- Muscle imbalances
- Breathing capacity
- Postural awareness
- Proper body mechanics
This helps them understand how the abnormal curvature affects your movement and daily life.
Treatment Plan & Pain Management
Each scoliosis patient receives a tailored treatment plan based on age, curve type, and skeletal maturity. For those with mild scoliosis, physiotherapy may be enough to manage scoliosis effectively. Complex cases might combine physiotherapy with bracing or surgery.
What Happens During Treatment
Generally, treatment sessions involve:
- Posture correction and education
- Breathing techniques and retraining to support lung function
- Schroth method exercises to de-rotate and stabilise the spine
- Muscle strengthening for the core and back
- Manual therapy (in some cases)
- Home-based scoliosis exercises for long-term maintenance
The therapist will also teach you to integrate proper posture and pain management strategies into daily routines.
Exercises for Scoliosis
Physiotherapy scoliosis-specific exercises are designed to address your unique spinal pattern. These may include:
- Schroth exercises: Targeted movements focusing on three-dimensional spinal correction and improved breathing
- Core stabilisation exercises for abdominal muscles
- Resistance training to build muscular symmetry
- Balance drills to enhance body awareness
- Mobility work to keep the spinal column flexible
These exercises for scoliosis can be modified as you progress for continuous adaptation and support.
Continuous Improvement
Scoliosis treatment isn’t a quick fix. Progress is gradual, especially in cases of moderate scoliosis or adult scoliosis. Regular monitoring, consistent home exercises, and physiotherapy sessions contribute to spinal health, long-term pain relief, and reduced reliance on invasive methods.
Other Forms of Treatment for Scoliosis
While physical therapy is beneficial, it’s not the only option. Depending on the severity and rate of curve progression, other treatments may be considered.
Braces
In growing adolescents, bracing helps prevent further progression of the curve. It’s often used alongside physiotherapy to reinforce posture and stability, especially in idiopathic scoliosis cases.
Surgery
Spinal fusion or scoliosis surgery may be recommended in severe scoliosis where non-surgical methods no longer manage symptoms or halt progression. However, even post-surgery, scoliosis physiotherapy plays a key role in rehabilitation, mobility restoration, and long-term function.
Conclusion
Scoliosis physiotherapy offers a non-invasive, practical approach to managing scoliosis effectively. With the right techniques, it can enhance mobility and promote spinal alignment. Regardless of the type you are diagnosed with, a structured physiotherapy plan can support pain reduction, posture correction, and overall well-being. While severe cases may require additional treatment options, physiotherapy remains a cornerstone of care for many scoliosis patients. It empowers you without compromising your quality of life.
Browse other articles by category
Physiotherapy for Knee Pain Physiotherapy For Slipped Disc Physiotherapy for Neck Pain PHYSIOTHERAPY
PHYSIOTHERAPY
 Hand Therapy
Hand Therapy
 Alternative
Alternative
 Massage
Massage
 Traditional Chinese Medicine Treatment
Traditional Chinese Medicine Treatment
 Rehab
Rehab
 Physiotherapy For Lower Back Pain
Physiotherapy For Shoulder Pain
Orthopedic Doctors, Insurance & Healthcare
Physiotherapy For Upper Back Pain
Frozen Shoulder
Physiotherapy for Back Pain
Physiotherapy For Lower Back Pain
Physiotherapy For Shoulder Pain
Orthopedic Doctors, Insurance & Healthcare
Physiotherapy For Upper Back Pain
Frozen Shoulder
Physiotherapy for Back Pain
 Whatsapp us now
Whatsapp us now